While large-scale events like Mission of Mercy provide critical access to care, they also reveal structural limitations, particularly in terms of clinical complexity, continuity, and sustainability. Community Vision Day was conceived to address these limits: a high-volume, community-focused clinic day hosted within the UPMC Vision Institute, leveraging existing infrastructure and supplies at minimal to no cost to patients, regardless of their insurance status.
Christened by UPMC CEO Leslie Davis and championed by UPMC Vision Institute Director José-Alain Sahel, UPMC Community Vision Day is the largest low-to-no-cost clinic program ever attempted within the UPMC ecosystem.
As program manager for CORAP, I led the Community Vision Day pilot end-to-end, including:
- Strategic planning and operational design
- Cross-departmental coordination and leadership alignment across UPMC
- Clinical workflow design tailored for high patient volume
- Volunteer recruitment, onboarding, and coordination
- Integration of insurance counseling and referral pathways
- Real-time operations, patient flow management, and issue resolution
- Post-event evaluation using patient and volunteer feedback
Operational success required buy-in from nearly every area of the Vision Institute, including physicians, advanced practice providers, technicians, opticians, security, concierge staff, translators, and community partners.
Community Vision Day represents a shift from episodic charity care toward sustainable, system-embedded access models. This initiative reflects my approach as a program leader: listening to feedback, recognizing structural limits, and designing care models that balance scale, dignity, and clinical excellence.
Based on the success of the pilot, Community Vision Day will be a quarterly event beginning in 2026 at the UPMC Vision Institute, with support from the Eye & Ear Foundation, UPMC Health Pan Social Impact & Community Engagement, and many other partners eager to close care gaps for our neighbors in need.
2026 UPMC Community Vision Days
Saturdays / 9AM-1PM
- February 21, 2026
- May 30, 2026
- August 22, 2026
- December 5, 2026
Patients are seen in order of appearance.
Learning & Program Evolution
Execution & Operations
The pilot relied on 75+ volunteers, including:
- Ophthalmologists and PAs
- Students and ophthalmic technicians
- Translators and security staff
- Opticians
- Representatives from UPMC Health Plan, SNAP, CORE, and PHAN
CORAP deployed volunteer training materials and scripts for multiple roles and scenarios to comply with UPMC’s anti-inducement language. Despite higher-than-expected demand (over 200 patients walked in or preregistered), the clinic successfully served 135 patients.
Patients represented a broad age range, from children to older adults, and most were uninsured or underinsured residents of nearby communities.
Clinical Complexity & Patient Need
Patients at the Community Vision Day Pilot presented with:
- Glaucoma
- Diabetic retinopathy
- Cataracts
- Dry eye disease
- Refractive error
- A rare case of cone-rod dystrophy
By hosting the event within the Vision Institute, providers had immediate access to diagnostic tools and clinical supplies, allowing higher-quality care than is possible in a temporary pop-up setting for high patient volumes, like Mission of Mercy.
Smaller-scale pop-ups, like our eyeVan Mobile Vision Clinics, do offer superb care in nontraditional clinic spaces, as do large-scale clinics that deliver high-volume glasses orders as opposed to comprehensive eye exams.
Continuity of Care & Equity
A core design principle of Community Vision Day was continuity, not just access.
The event gives patients the opportunity to easily access continued care by providing insurance counseling, referral pathways for specialty follow-up appointments, and connections to ongoing care within the UPMC system.
Metrics & Outcomes
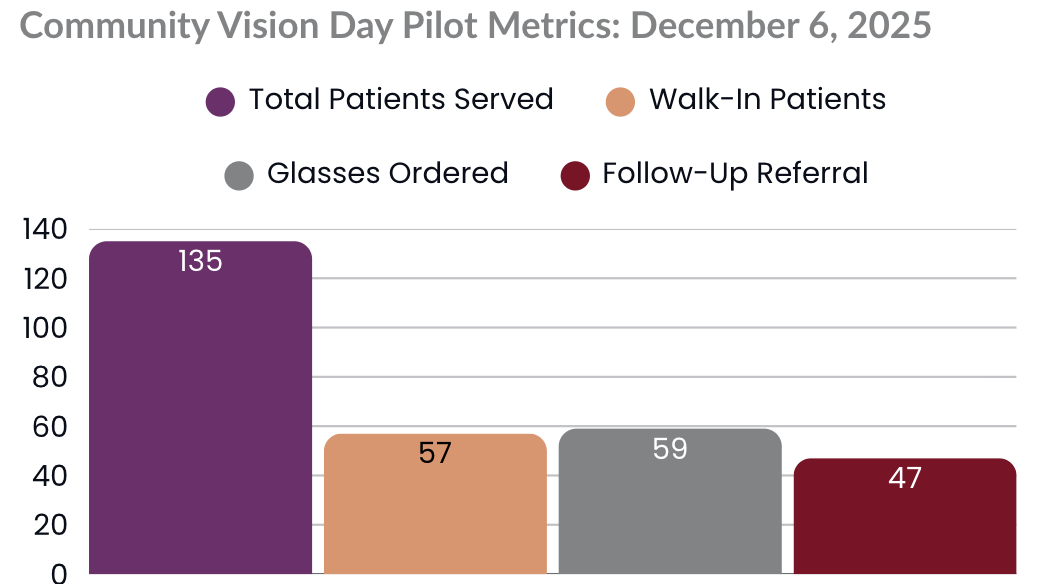
- 135 patients served, including 15 children
- Majority uninsured and from the surrounding neighborhoods
- High clinical complexity managed safely and effectively
- Strong volunteer engagement and cross-departmental collaboration
- Positive patient and volunteer feedback
The pilot validated:
- Significant community demand
- Clinical appropriateness of a clinic-based access model
- Operational feasibility with the right planning and leadership