Mission of Mercy is a large-scale, two-day charitable healthcare event offering free dental, hearing, and vision services to thousands of uninsured and underinsured patients. The Vision Services section operates as a fully functional pop-up eye clinic, requiring coordination of clinical staff, imaging equipment, electronic medical record access, optical services, and volunteer teams under tight space, time, and staffing constraints.
In both 2024 and 2025, I served as the primary point of contact and section lead for Vision Services, acting simultaneously as program manager, operations lead, and clinical workflow designer.
Role & Scope
In 2024, Mission of Mercy (November 1-2, 2024) was my primary project shortly after onboarding in September; by 2025, I led the Mission of Mercy event (October 24-25, 2025) as the fully realized program manager for UPMC’s mobile vision clinics and remote access initiatives, including device trials supporting ophthalmology telehealth.
Management of both Mission of Mercy Events involved end-to-end oversight of every operational facet of the Vision Section:
- Clinical workflow design and triage protocol development
- Recruitment, onboarding, scheduling, and management of 175+ volunteers, including students, interns, and clinical staff
- Development of training materials and volunteer documentation
- Coordination with Mission of Mercy operations team
- Equipment delivery, setup, teardown, and electrical planning—including integration of the mobile eyeVan
- Real-time crowd management, patient flow control, and issue resolution for 12-hour event days
- Troubleshooting EPIC access and permissions across shared devices provided by Mission of Mercy
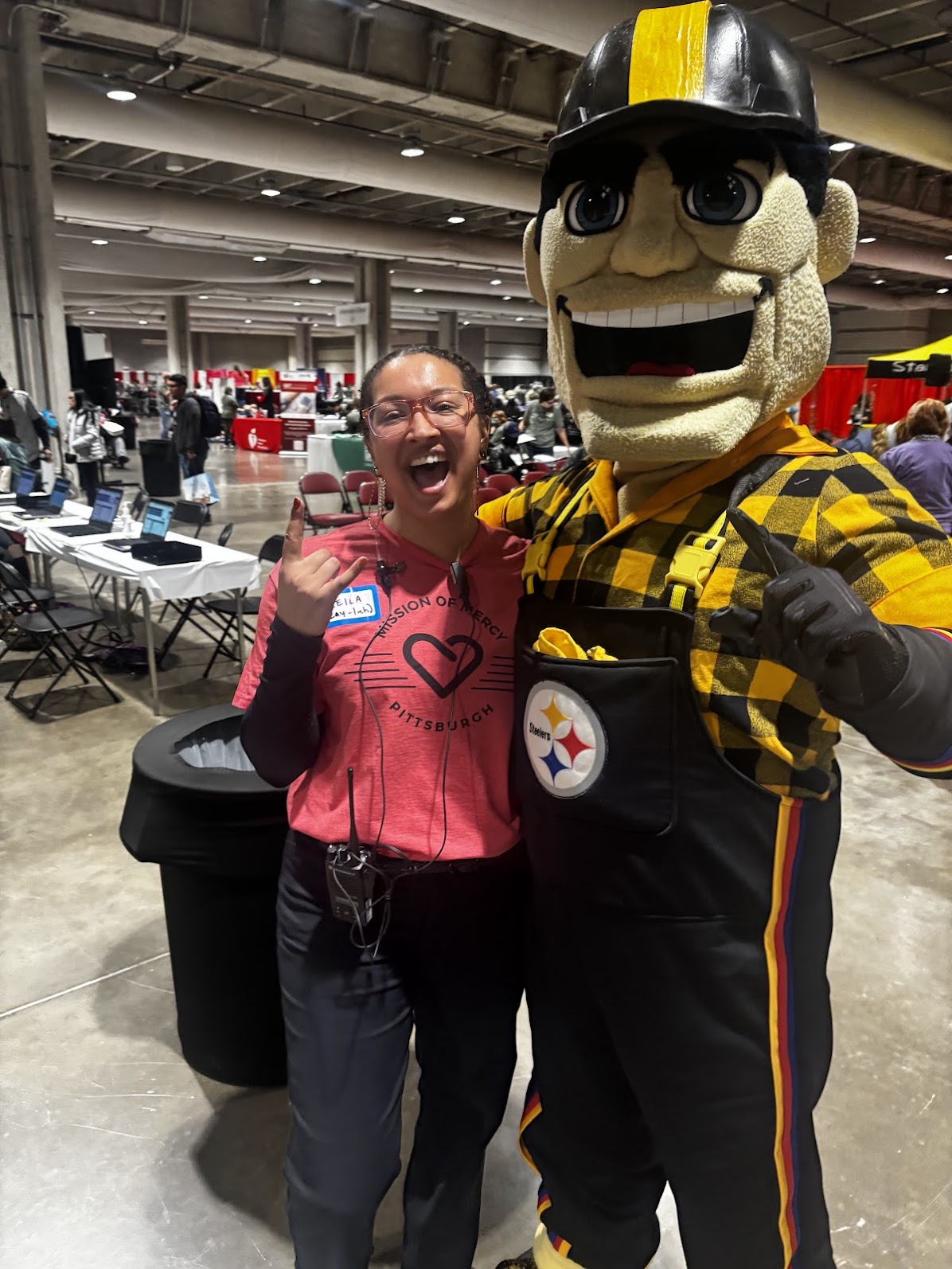
- Media engagement and relationship-building with community partners supporting the event
- Determining patient intake cutoffs to balance patient access with quality and teardown timelines
Metrics
Learning & System Evolution
Challenges Identified (2024)
The 2024 event surfaced several critical constraints:
- Patient flow bottlenecks, particularly at optical services and comprehensive exams
- Congestion in the retinal imaging area, as most patients requiring comprehensive exams also require retinal imaging
- Confusion among patients regarding the next clinical steps
- Digital patient tracking system failure within the first hour
- Late volunteer onboarding and inconsistent communication
- Underutilized clinic space limiting throughput and waiting capacity
When the digital tracking system provided by MOM operations failed, we immediately pivoted to whiteboards and paper tracking to maintain continuity of care, ensuring patients were still seen safely and efficiently.
Interventions & Redesign (2025)
Using feedback from patients, volunteers, and internal debriefs, I led a series of targeted improvements for 2025:
Clinical Workflow & Triage
- Created a separate imaging area to relieve congestion in comprehensive exams
- Increased ophthalmic technician staffing for imaging and triage
- Implemented an exam passport signed at each station to clarify patient progression and reduce confusion
- Introduced a five-minute limit for glasses selection to improve fairness and throughput
Operations & Space Design
- Increased and reorganized waiting areas across stations
- Expanded clinic footprint within the convention center
- Built dedicated checkout area in a previously underutilized space
Volunteer Systems
- Launched volunteer recruitment earlier than in 2024
- Updated information architecture of volunteer registration portal
- Distributed training materials and role guides well in advance
- Assigned section leads to manage breaks, questions, and escalation
- Built and managed a two-shift schedule spanning 5:00 AM–5:00 PM across both days
Tracking & Metrics
- Replaced fragile digital tracking with a clipboard stacking system, improving reliability and real-time visibility
- Improved service quantification, enabling cost estimation of delivered free care
Partnerships & Innovation
- Continued partnership with Topcon, with a more targeted approach in 2025
- Trialed devices aligned with long-term integration into mobile vision clinics and teleophthalmology workflows
Mission of Mercy demonstrated both the power and the limits of large-scale pop-up clinics. While the event delivers extraordinary access, feedback, and observation highlighted that quality of care would improve in established clinical environments.
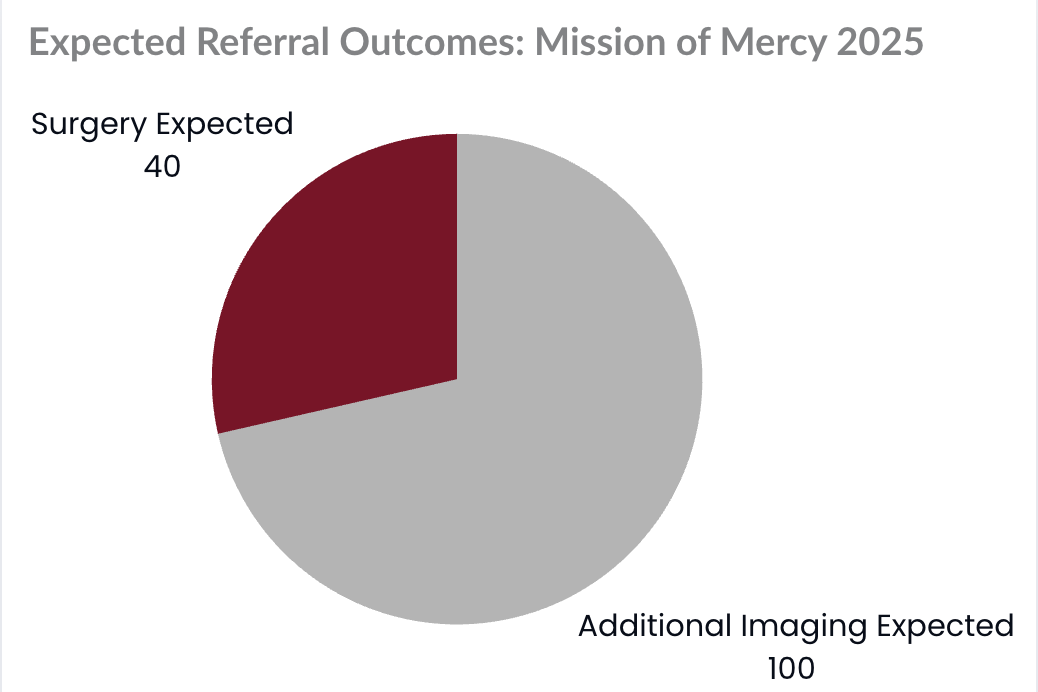
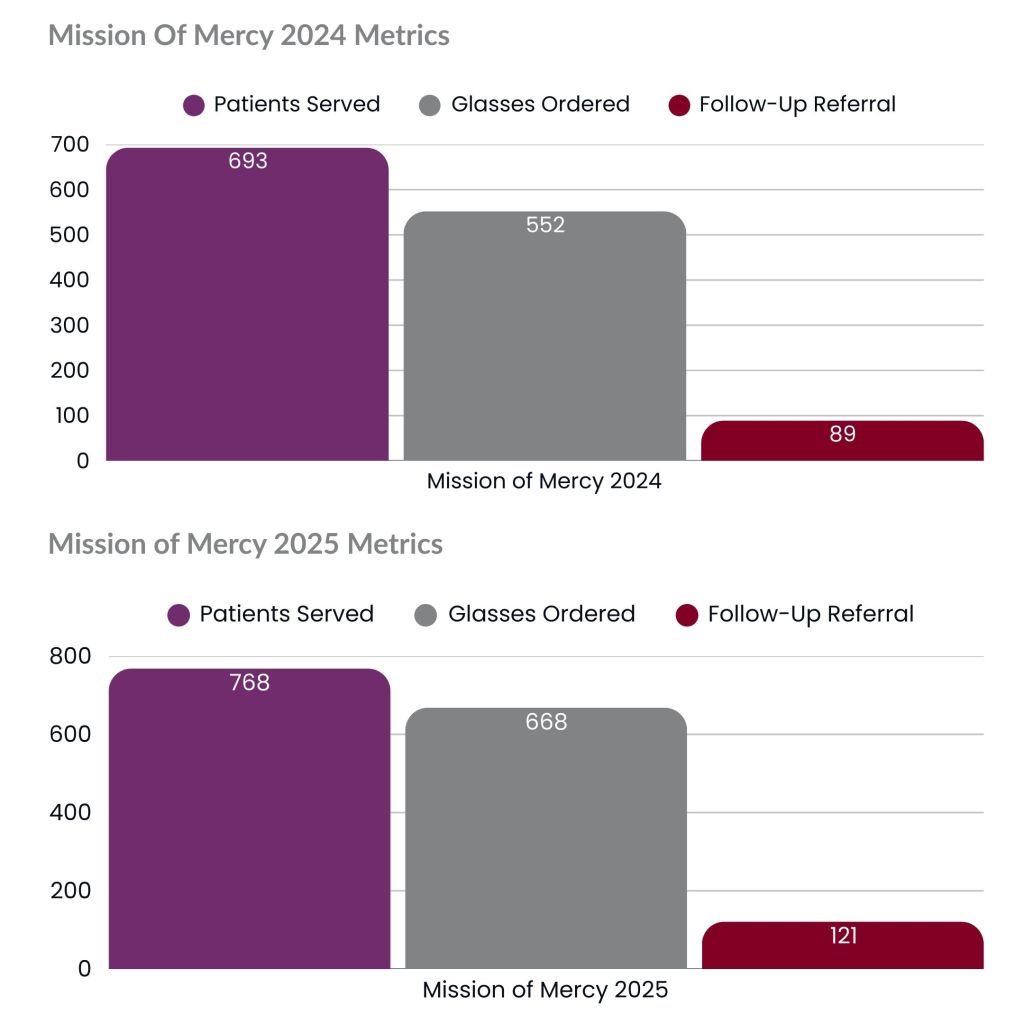
- Year-over-year impact:
- Nearly 100 additional patients served
- Improved patient clarity, flow, and experience
- Higher volunteer satisfaction and confidence
- Stronger continuity of care through structured referrals
Patients from both events were referred for follow-up care as needed, including uninsured patients. Insights from Mission of Mercy directly informed a strategic shift toward replicable workflows supporting mobile clinics and telehealth programs, and expanded care delivery within the UPMC Vision Institute with Community Vision Day.
In 2025, we established Community Vision Day as a formal referral pathway, allowing patients to access low- or no-cost specialty follow-ups beyond Mission of Mercy.
This work reflects my approach as a program leader and systems builder: leading with dignity under pressure, translating chaos into resilient workflows, and designing models of care that can scale without compromising patient experience or clinical quality.